 High-quality endoscope reprocessing is paramount for patient safety, but hospitals must also make sure that they are being efficient in reprocessing to maintain a profitable operation. Many patient safety hazards can occur if a single process is skipped or mishandled, so hospitals must be thorough in their processes. As hospitals are continually trying to find new ways to become more efficient, staff are also being pushed to increase reprocessing quality while reducing their reprocessing times. While these priorities are often at odds, here is how one major hospital accomplished exactly this feat.
High-quality endoscope reprocessing is paramount for patient safety, but hospitals must also make sure that they are being efficient in reprocessing to maintain a profitable operation. Many patient safety hazards can occur if a single process is skipped or mishandled, so hospitals must be thorough in their processes. As hospitals are continually trying to find new ways to become more efficient, staff are also being pushed to increase reprocessing quality while reducing their reprocessing times. While these priorities are often at odds, here is how one major hospital accomplished exactly this feat.
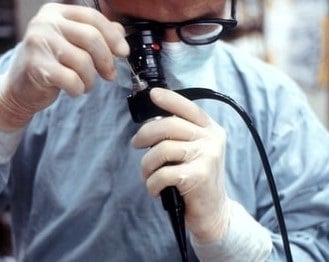
A major academic medical center in Pennsylvania has been using Mobile Aspects’ endoscope tracking system to electronically capture all endoscope reprocessing and storage transactions for several years. They initially acquired iRIScope to meet and exceed The Joint Commission (TJC) regulations around endoscope documentation and clean storage. Mobile Aspects’ iRIscope smart cabinets and reprocessing software capture critical scope data points. Utilizing the data from iRIScope, hospital staff can learn all the details about a scope’s lifecycle – for instance who removed the scope, what procedure it was used in, when the scope was removed and cleaned, etc. This helped the hospital to understand the various bottlenecks its scopes were facing during their lifecycle.
In addition, the hospital started to notice other variables that were causing problems for hospital staff while managing their scopes. Scopes were often used on weekends or by other departments. In these cases, it was difficult for the hospital staff to figure out the location and status of a scope after a procedure. This reduced the availability of scopes when they were critically needed for the next procedure.
In order to reduce their bottlenecks and create a more efficient reprocessing cycle, the hospital analyzed the timestamp data coming out of iRIScope. Based on the data, they were able to find inefficient staff members and offer training and retraining to improve reprocessing efficiency. They were also able to identify which steps were taking the most time to complete and further reduce bottlenecks by making sure scopes didn’t linger in any step for too long. Using this data, the hospital was able to reduce the average reprocessing cycle to less than an hour for pre-cleaning and high-level disinfection.
Another large bottleneck that the hospital identified was the time it took for scopes to be transported – both between procedure rooms and sterile processing (SPD) and between SPD and clean storage. The data was showing that the time it was taking for scopes to arrive back in SPD after a procedure was as long as 10 to 12 hours. After each scope completed its high-level disinfection, it was taking up to another 5 hours just to reach clean storage. Once these bottlenecks were identified, the hospital was then able to work with Mobile Aspects to reduce these turnaround times. For example, the hospital implemented alerts that were sent if the staff were not able to return the scope to clean storage within 4 hours of high-level disinfection.
By chipping away at these inefficient processes, the hospital was able to dramatically decrease the average turnaround time between when a scope was removed from a clean storage cabinet for a procedure and when it was returned to clean storage after reprocessing. The turnaround time was reduced by over 50%, from just over 10 hours to just under 5 hours on average. This reduction led to an increase in availability of scopes, which reduced procedure delays or cancellations and increased the overall profitability of their endoscopy practice.
